Wrong way round
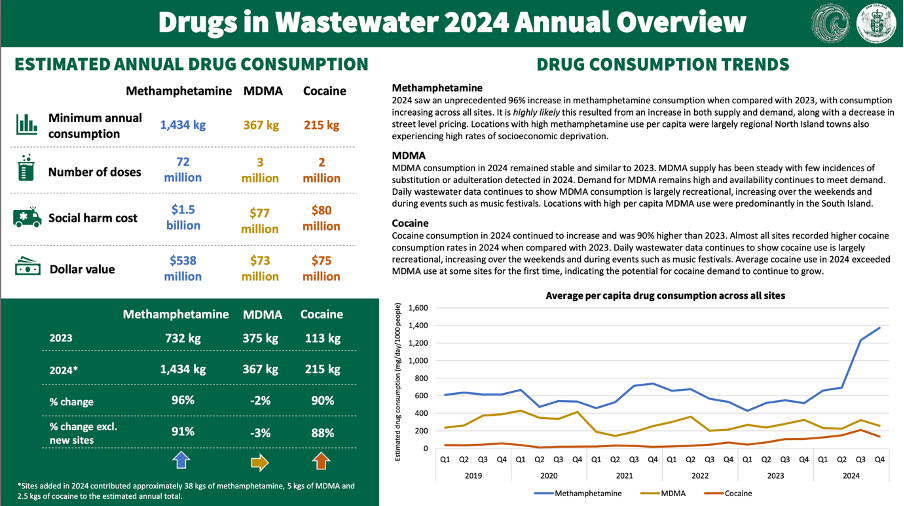
As a country, we have had a seismic shift in methamphetamine supply and consumption. We are consuming twice what we were a year ago, and that seems to now be our new normal. This is despite record drug busts and seizures. In my role as the Executive Director of the New Zealand Drug Foundation, it is agonising how difficult it is to get an investment in treatment, prevention and harm reduction despite it being so evidently needed and despite the enormous harm to the community from failing to act.
War on drugs has demonstrably failed
Fifty years on, it is crystal clear the war on drugs has failed by any measure. We have record-breaking consumption of methamphetamine and cocaine. Our drug supply is volatile and more potent than ever before. There is the constant threat of potent opioids like fentanyl and nitazenes entering the drug supply, and which have already claimed the lives of New Zealanders. And we have new and novel psychoactive substances being created all the time as the illicit markets try to evade law enforcement.
By choosing a ban and police model in the 1960s and 70s, we chose to abandon regulatory tools we might have been able to deploy and we gave control over the drug supply to the illicit market.
While drug busts and seizures can have complex impacts (e.g. the market might meet the unmet demand with novel and more dangerous substances), I am grateful that the vast quantities being seized at the border and by police raids haven’t made their way into the community. The famed 2022 Comancheros bust alone was 613kg of methamphetamine, which is a volume that is approximately what all of New Zealand would consume in a year at pre-2024 levels.
But while we have gotten tougher on crime over the last couple of years, and made record-breaking seizures, you wouldn’t know it had ever happened looking at the wastewater results, which show record-breaking consumption of both methamphetamine and cocaine.
Worse than busts and seizures not working, they are akin to burning tax dollars if we don’t do demand-side measures alongside them.
As a country, we’ve been heavily reliant on supply-side interventions. The bulk of the resource is going into policing and customs seizures.
However, in a market where there’s demand for a lucrative product, if the supplier disappears, a new supplier pops up. So when a drug bust happens, and one supplier is taken out, someone else steps in to meet the unmet demand. This is particularly true where there is addiction involved.
Reports of harm are really worrying
The regions most affected, based on wastewater information via the police, are Northland, Tāmaki Makaurau, Eastern and Waikato. That’s not to say other places don’t have meth use—methamphetamine, like other drugs, is used across society—but it’s true to say harm tends to be more concentrated in lower socioeconomic groups.
I have been up to Northland, Muriwhenua and Whangārei in particular. And my team and I are talking to people from around the four regions to get a sense of what is happening. And what they need.
I have heard from them terms like ‘epidemic’ and gotten a sense of extreme overwhelm from very seasoned and capable professionals.
Overall, they report a lack of access to help. And a need for more prevention work. I have also heard about and witnessed a range of unmet social, economic and health needs exacerbating, if not fuelling, matters.
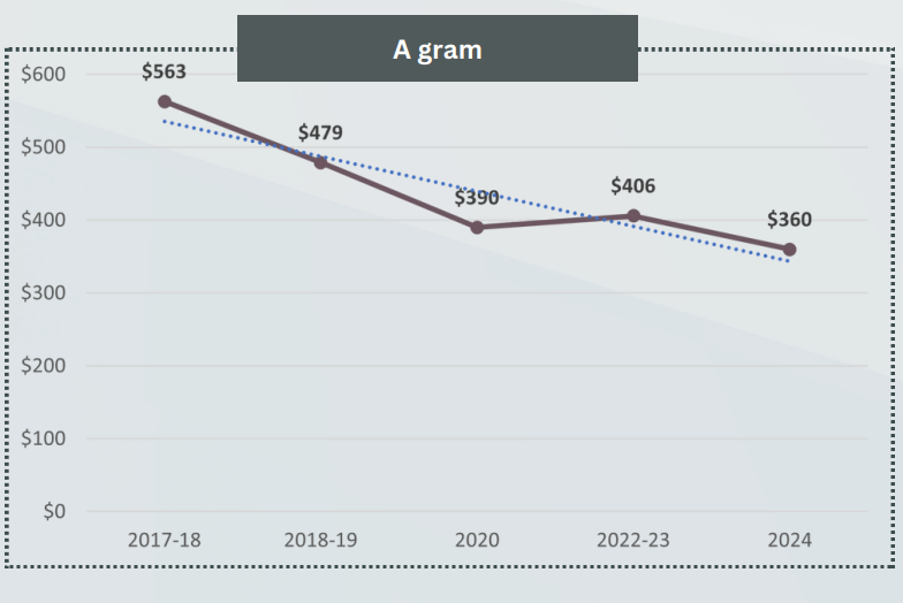
We’ve had reports out of some addiction services saying the amount people are consuming has vastly increased. One reported as much as a gram a day. We’re hearing about increased frequency of use at our drug checking clinics.
We have had shifts in organised crime in New Zealand, and a growing supply of methamphetamine into the country.
Bold action is long overdue
I would like to get the following quote from a recent report from the Government’s Ministerial Advisory Group on Transnational, Serious and Organised Crime put onto a T-shirt. Or perhaps some well-placed billboards. They described our current approach as akin to “rearranging deck chairs on the Titanic” and said that “it will take new ways of thinking, and bold changes, to alter the course for New Zealand.”
The boldest action would be law reform, which is overdue and necessary but unlikely.
Massively scale up help and prevention efforts
Several weeks ago, Minister Doocey hosted us and about 200 people from the sector in a summit to strengthen addiction and harm reduction responses. We discussed a range of challenges including the changed drug supply. And participants shared their thoughts about what was needed, which we have taken forward to the Minister and Ministry. These things also fit with the evidence:
A rapid escalation of addiction treatment, including investment in accessible community-based, peer-led mutual aid like SMART Recovery
- Revamping and expanding proven health-based responses like Te Ara Oranga. If we had gotten in and invested in the development and expansion of the Northland Police-led health-based approach, we might not be in such a dire place now. It needs reinvigorating and expansion. And it needs a revamp to address some criticism of this programme not being adequately connected to mana whenua in the areas it covers. Key personnel have also moved on, so a regrouping of the right people and approach are also vital.
- A campaign that reduces stigma and encourages people to have conversations about their use with loved ones and to access help
- Ramping up prevention by tackling unmet health needs by:
- offering better support and treatment for people who use methamphetamine and have ADHD (one Australian study showed 45% of people who use illicit stimulants regularly screened positive for ADHD
- investigating medication-assisted treatment options for people with methamphetamine dependence
- Increasing harm reduction service availability, for example access to sterile injecting equipment to prevent communicable disease impacts
- More kaupapa Māori-driven health responses – much more.
ADHD treatment could be the added bold action that makes a dent in demand
It is thought that about half of people who take illicit stimulants have untreated ADHD. One study in Australia showed 45% of people who use illicit stimulants screened positive for ADHD, and other international studies essentially back that up.
We think there’s a big opportunity to address methamphetamine use by helping people who are using—or starting to experience problems—with the opportunity to be screened, diagnosed and treated for ADHD. That could help people have more control over their lives and other health issues—not just methamphetamine use—be able to have a prescription where that’s relevant and appropriate, get off illicit supply, and … that might actually make a dent in demand.
Under-resourced and a disconnected system
Being pragmatic, we keep trying to dream up ways to make it more cost-effective for government, given the cost pressures on the system at the moment. And we need to value addictions and harm reduction properly and invest in them in a way that doesn’t mean we are wasting other spending.
But it’s clear that while we under-invest in Health and instead invest in supply-side Police/Customs interventions – we are wasting tax dollars anyway.
The addictions and harm reduction sector is vastly under-resourced. We receive about 11% of the mental health ringfence. And the 2019 Wellbeing Budget had a big uplift for mental health, but addictions got around 3% of that uplift—and most of it went to directly employed Te Whatu Ora, not the community NGO sector.
Comparisons to what we spend on Police and other Justice interventions make the under-investment in Health crystal clear.

We do have some hope. And hope is needed, because we may be witnessing one of the most serious changes to our drug supply that has happened in decades. Bold action and a rebalance are very overdue and badly needed.